The Science Blog
How to Revolutionise Healthcare with Nanomedicine
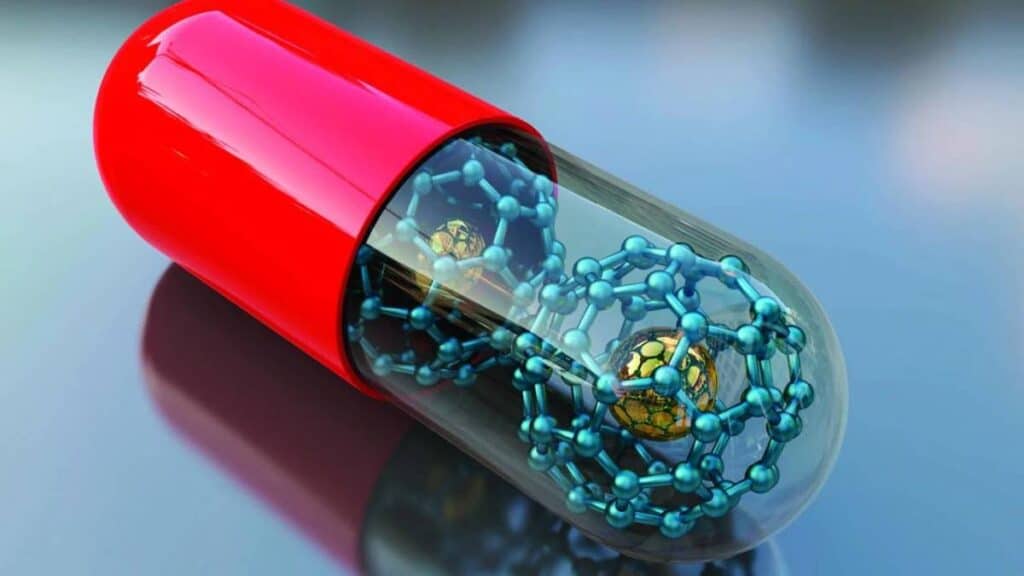
In the changing world of healthcare, nanotechnology is making a big difference. This is especially true in the growing field of nanomedicine. This new method uses tiny particles to change how we diagnose, treat, and prevent diseases. Nanomedicine was once just a sci-fi idea. Now, it’s real and offers better treatments and improved patient outcomes.
Nanomedicine stands out by enabling targeted drug delivery, pre cision treatment, and innovative diagnostics. Through nanoparticles, medical professionals can combat diseases with unprecedented accuracy and efficiency. This guide looks at nanomedicine. It covers its real-world uses and what it could mean for healthcare in the future.
Quick Guide: Revolutionising Healthcare with Nanomedicine
- Nanomedicine leverages tiny particles to transform healthcare, offering targeted drug delivery, personalised treatments, and advanced diagnostic tools.
- By working at the nanoscale, it enables more precise, efficient, and safer treatments, especially in cancer, neurodegenerative diseases, and regenerative medicine.
Why Nanomedicine Matters
Transforming Traditional Treatments
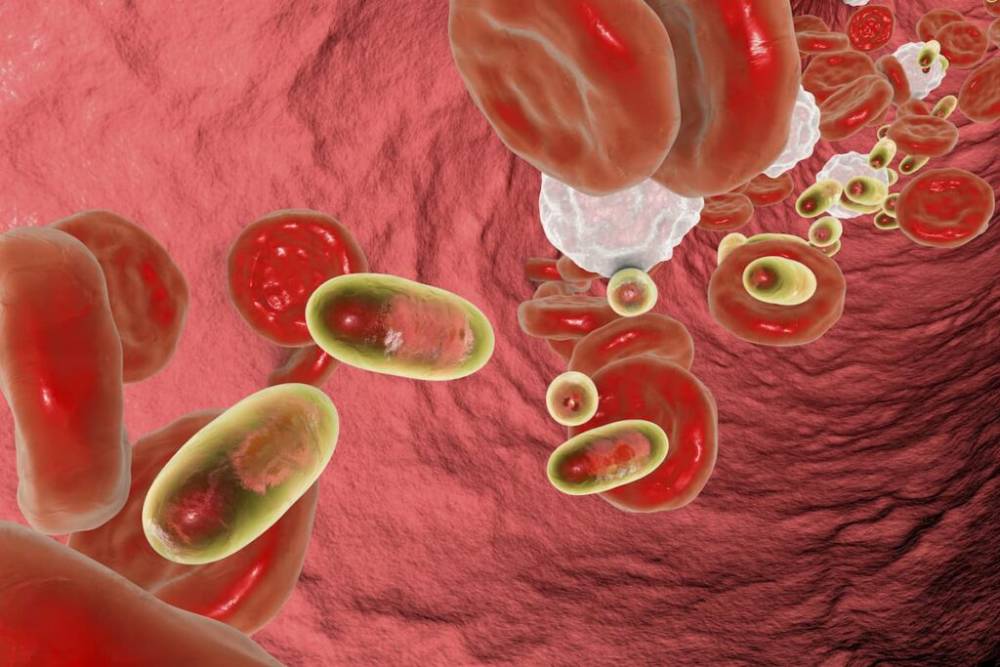
Nanomedicine is more than a technological advancement. It represents a fundamental shift in how we approach medical treatments. Traditional therapies like chemotherapy and systemic drugs can harm both sick and healthy cells, causing serious side effects. Nanomedicine offers targeted treatments. These treatments protect healthy cells, which boosts effectiveness and lowers complications. This new method helps a lot in cancer treatments. Now, chemotherapy drugs can go straight to tumour cells.
Expanding Applications Beyond Cancer
While cancer treatment is a major area of nanomedicine, its applications extend far beyond oncology. Nanotechnology is being utilized in cardiology, infectious diseases, regenerative medicine, and neurology. Nanoparticles can now cross the blood-brain barrier. This creates new ways to treat neurodegenerative diseases such as Alzheimer’s and Parkinson’s. Nanoscale scaffolds are changing tissue regeneration. They speed up healing for injuries and chronic wounds.
Pro Tip: Nanomedicine thrives on customization. Tailoring treatments to individual patient needs, based on genetic and disease profiles, maximises effectiveness and reduces side effects.
How Nanomedicine Works: Step-by-Step Guide
1. Understanding Nanoparticles
What Are Nanoparticles?
Nanoparticles are incredibly small structures, measuring between 1 and 100 nanometers. To put this into perspective, a nanometer is one-billionth of a meter—about 100,000 times smaller than the diameter of a human hair. Their minuscule size allows them to interact with biological molecules within cells. This makes them ideal for targeted drug delivery and precision medicine.
Engineering Nanoparticles
You can design nanoparticles to improve their size, shape, and surface features for medical purposes. Scientists can design them to:
- Carry specific drugs or therapeutic agents
- Target and bind to specific diseased cells
- Respond to stimuli within the body, such as pH changes or heat
This customisation helps create effective treatments designed for each patient.
2. Implementing Nanomedicine in Healthcare
Targeted Drug Delivery
A cornerstone of nanomedicine is its ability to deliver medication precisely where it’s needed. Coating nanoparticles with ligands helps them find specific cell receptors. This way, drugs can be released right at the disease site. This precision reduces systemic exposure and minimises side effects.
Precision Medicine & Personalized Treatments
Nanomedicine allows for personalised treatments. It takes into account a person’s genetic profile, disease traits, and how they respond to treatment. This is particularly valuable in oncology, where tailored therapies significantly improve outcomes.
Advanced Diagnostic Tools
Beyond treatment, nanotechnology is revolutionising diagnostics. Nanosensors and imaging agents allow for early disease detection, even before symptoms manifest. For example:
- Gold nanoparticles are used in imaging techniques to enhance cancer detection.
- Quantum dots provide real-time visualisation of cellular processes.
Early detection translates to better treatment success rates and improved patient prognoses.
Important: While nanomedicine holds great promise, ongoing research, safety testing, and ethical considerations are crucial to ensure its long-term success and widespread application.

Case Studies & Real-World Applications
1. Cancer Treatment Breakthroughs
A significant breakthrough in nanomedicine has been its role in oncology. Clinical trials show that nanoparticle-based chemotherapy drugs boost survival rates and lower side effects. For example:
- Liposomal Doxorubicin (Doxil): This nanomedicine helps deliver drugs to tumours better. It also reduces heart-related side effects.
- Abraxane is a nanoparticle form of paclitaxel. It helps the drug dissolve better. This improves treatment results for patients with breast and pancreatic cancer.
2. Fighting Neurodegenerative Diseases
A big challenge in treating brain disorders is the blood-brain barrier. It stops most drugs from getting to the brain. Nanomedicine has addressed this issue by creating nanoparticles capable of crossing this barrier. Researchers are now developing nanotherapeutics for:
- Alzheimer’s disease: Nanoparticles carrying neuroprotective agents can slow disease progression.
- Parkinson’s disease: Targeted delivery of dopamine-releasing nanoparticles is showing promising results.
3. Revolutionary Wound Healing & Regenerative Medicine
Nanomedicine is playing a pivotal role in regenerative medicine. Nanoscale scaffolds and nanofiber dressings help tissue regeneration. They support cell growth and lower the risk of infection. This innovation is particularly beneficial for:
- Burn victims
- Patients with chronic wounds, such as diabetic ulcers
Common Mistakes & Misconceptions
Mistake 1: Assuming Nanomedicine is a “Magic Bullet”
While nanomedicine holds immense promise, it is not a universal cure-all. Each disease and patient requires a tailored approach, and ongoing research is crucial to refine treatments.
Mistake 2: Overlooking Safety & Ethical Considerations
Despite its benefits, nanomedicine raises safety concerns. The long-term effects of nanoparticles in the body are still being studied. This requires careful testing and ethical considerations.
Mistake 3: Underestimating Scalability Challenges
Nanoparticles work well in labs, but making them for widespread clinical use is tough. Researchers are working to overcome manufacturing and cost barriers.
Frequently Asked Questions (FAQ)
Is nanomedicine safe?
Yes, but it requires extensive testing. Regulatory bodies such as the FDA and EMA oversee nanomedicine trials to ensure safety and efficacy before approval.
How does nanomedicine differ from traditional treatments?
Nanomedicine provides targeted treatment and has fewer side effects than traditional therapies. This makes it more efficient for managing diseases.
Can nanomedicine cure cancer?
Nanomedicine doesn’t cure cancer, but it makes treatment much better. It improves how drugs are delivered, boosts their effectiveness, and lessens side effects.
How soon will nanomedicine become mainstream?
Many nanomedicine-based treatments are already in clinical use. However, widespread adoption depends on further research, regulatory approvals, and cost reductions.
What are the ethical concerns with nanomedicine?
Concerns include potential toxicity, long-term health effects, and accessibility. Ethical considerations focus on ensuring the safety and equitable distribution of treatments.
The Future of Nanomedicine
Nanomedicine represents a bold leap forward in revolutionising healthcare. Using nanoparticles boosts disease treatment, sharpens diagnostics, and leads to more personalised, effective care. As the field grows, scientists, clinicians, and policymakers must work together. This teamwork is key to maximising potential and tackling safety and ethical issues.
Nanomedicine shows a future in healthcare where diseases are managed with great precision, not just treated. The question is no longer whether nanomedicine will transform healthcare—it’s how far it will take us.
Stay updated on the latest in nanomedicine. Think about how you can help in this exciting area. The future of healthcare is in our hands, whether you’re a researcher, clinician, or just curious.









